Surgery may be the answer when all else fails. This was the message presented by Dr. Prayuth Diloksampant during his presentation concerning obesity and the surgical options available to those affected at the Sunday, February 19 meeting of the Pattaya City Expats Club. He pointed out that being seriously overweight often leads to serious medical problems.

Dr. Prayuth from Bangkok Hospital Pattaya received his MD from Chulalongkorn University in 1987 and his certification by the Thai Board of General Surgery, Ministry of Public Health, in 1991. He attended Laparoscopic surgery workshops for Bariatric and Colorectal surgery in 2006, as well as a training course in Bariatric Surgery in Switzerland. He has also advanced his studies in China, Vietnam, and Taiwan.
From 1987 to 1991 he did his Internship in Haadyai general hospital, Songkhla, Thailand and was on the surgical staff in Haadyai general hospital from 1991 to 1993. From 1993 to 2003 he was a general surgeon at Samithivej and Phyathai hospital in Sriracha, Chonburi. He is presently with the Surgery Center in BHP specializing in advanced laparoscopic surgery and bariatric surgery.
The doctor explained that the major emerging threat to public health in Europe is excessive body weight and obesity. These conditions are no longer an individual health-related problem but a public health problem. Over two thirds of the U.S. population is overweight and half of the overweight population is obese. Over 1.7 billion people, worldwide, have these weight problems.
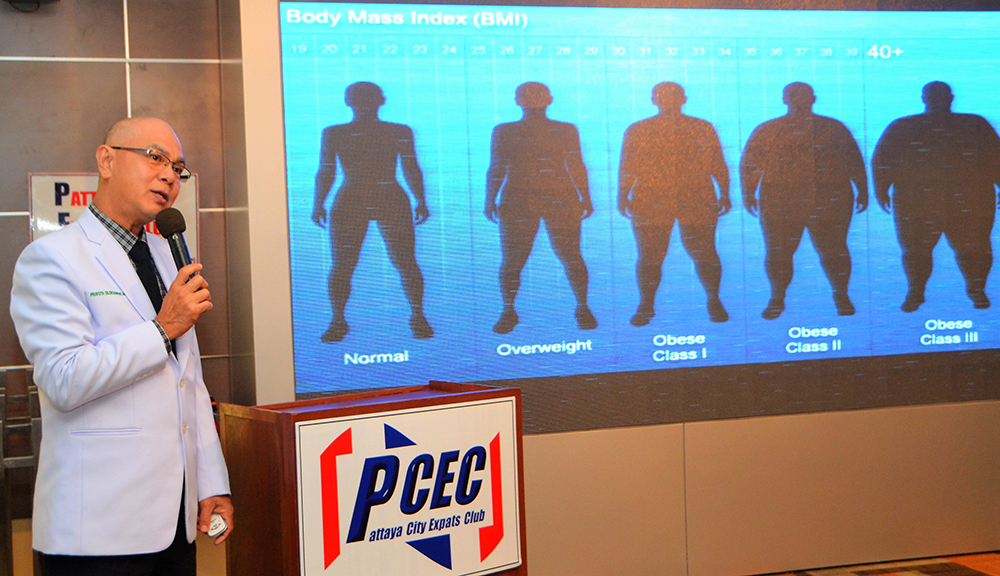
To determine if a person is underweight, normal, overweight or obese, the Body Mass Index (BMI) or Quetelet index, is used. It is calculated by determining the mass (weight) and height of an individual. The BMI is defined as the body mass (measured in kilograms), divided by the square of the body height (measured in meters) and is universally expressed in units of kg/m2. The BMI is an attempt to quantify the amount of tissue mass (muscle, fat, and bone) in an individual and then categorize that person as underweight, normal weight, overweight, or obese, based on that value.
However, there is some debate about where on the BMI scale the dividing lines between categories should be placed. Commonly accepted BMI ranges are underweight: under 18.5 kg/m2, normal weight: 18.5 to 25, overweight: 25 to 30, obese: over 30. People of Asian descent have different associations between BMI, percentage of body fat and health risks than those of European descent, with a higher risk of type 2 diabetes and cardiovascular disease. There are three classes of obesity, 1 – moderate, 2 – severe and 3 – very severe. Morbidity of obesity is associated with diabetes, high blood pressure, hyperlipidemia, joint pain, obstructive sleep apnea, cancer and depression. The doctor mentioned several surgical options.

Laparoscopic Surgery – Also called minimally invasive surgery (MIS) or band aid surgery, is a surgical technique in which operations are performed through small incisions (usually 0.5–1.5 cm) in various locations on the abdomen. The abdomen is usually insufflated with carbon dioxide gas and graspers, scissors, clip applier are used to remove the fat cells. The most significant risks are from injuries during tool insertion, umbilical hernias, umbilical wound infection, and penetration of blood vessels or penetration of the small or large bowels. Also, malnutrition issues can develop. Mortality is about 1% and surgical failure is also 1%, so the success rate is 98%.
Gastric Band – The surgeon inserts an adjustable gastric band through a small, 1.25 cm, incision near the belly button. The band is placed around the upper part of the stomach to create a smaller stomach pouch. This slows and limits the amount of food that can be consumed at one time. As patients lose weight, the bands will need adjustments, or “fills”, to ensure comfort and effectiveness. The gastric band is adjusted by introducing a saline solution into a small access port placed just under the skin. The average gastric banding patient loses 500 grams to a kilogram (1–2 pounds) per week, consistently, but heavier patients often lose faster amounts in the beginning.
Rou-en-y Gastric Bypass (RNY) – This refers to a surgical procedure in which the stomach is divided into a small upper pouch and a much larger, lower “remnant” pouch and then the small intestine is rearranged to connect both. This leads to a marked reduction in the functional volume of the stomach, accompanied by an altered physiological and physical response to food. The operation is prescribed to treat morbid obesity. The long-term mortality rate of gastric bypass patients has been shown to be reduced by up to 40%.

Sleeve Gastrectomy -The part of the stomach, along its greater curve, is resected. The stomach is “tubulized” with a residual volume of about 150 ml. This volume reduction provides the food intake restriction component of this operation. This type of gastric resection is anatomically and functionally irreversible. The stomach is then disconnected from the duodenum and connected to a section of the small intestine, situated away from the point of origin. The duodenum and the upper part of the small intestine are reattached to the rest at about 75–100 cm from the colon.
In conclusion, the after-operation weight loss can be in the range of 60% to 70% of the excess body weight. The patient can resume a normal diet and will regain strength as the weight drops. Weight loss, depending on the procedure and patient’s weight, can take about one to two years.
After Dr. Prayuth answered several questions from the audience, MC Roy Albiston brought everyone up to date on Club activities and was followed by the Open Forum, where questions are asked and answered or comments made about Expat living in Pattaya. For more information about the PCEC, visit their website at www.pcecclub.org.




