Washington (AP) – Alternating the promise of cures for intractable diseases with anxiety about designer babies and eugenics, hundreds of scientists and ethicists from around the world began debating the boundaries of a revolutionary technology to edit the human genetic code.
“We sense that we are close to being able to alter human heredity,” Nobel laureate David Baltimore of the California Institute of Technology said Tuesday, Dec. 1 in opening an international summit to examine what he called “deep and disturbing questions.” ‘’This is something to which all people should pay attention.”
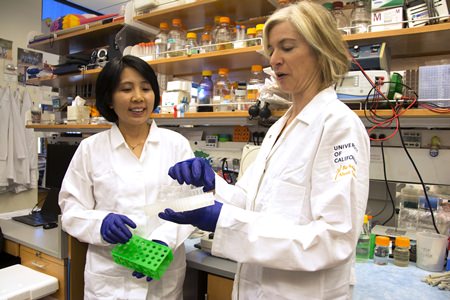 In this photo provided by UC Berkeley Public Affairs, taken June 20, 2014, Jennifer Doudna, right, and her lab manager, Kai Hong, work in her laboratory in Berkeley, Calif. (Cailey Cotner/UC Berkeley via AP)
In this photo provided by UC Berkeley Public Affairs, taken June 20, 2014, Jennifer Doudna, right, and her lab manager, Kai Hong, work in her laboratory in Berkeley, Calif. (Cailey Cotner/UC Berkeley via AP)
It’s an issue that gained urgency after Chinese researchers made the first attempt at altering genes in human embryos, a laboratory experiment that didn’t work well but did raise the prospect of one day performing genetic engineering that goes far beyond helping one sick person – and could pass modified genes on to future generations.
“This is a technology that could have profound implications for permanent alteration of the human genome,” molecular biologist Jennifer Doudna of the University of California, Berkeley, wrote this week in the journal Nature. Doudna co-invented the most-used gene-editing tool, and her calls for scientists, policymakers and the public to determine the right balance in how it’s eventually used led to this month’s gathering.
At issue are tools to edit precisely genes inside living cells, finding specific sections of DNA to slice and repair or replace, much like a biological version of cut-and-paste software. There are a few methods but one with the wonky name CRISPR-Cas9 is so fast, cheap and simple for biologists to use that research is booming.
Scientists are engineering animals with humanlike disorders to unravel the gene defects that fuel them. They’re developing potential treatments for muscular dystrophy, sickle cell disease and cancer. They’re trying to grow transplantable human organs inside pigs. They’re even hatching mutant mosquitoes designed to be incapable of spreading malaria, and exploring ways to wipe out invasive species.
Twice, experimental gene-editing therapies have been tried in people: British doctors treated a 1-year-old with leukemia with donated immune cells altered to target her cancer, and a California company is testing a way to make HIV patients’ own immune cells better resist the virus.
One hurdle is safety. While the CRISPR tool is pretty precise, it sometimes cuts the wrong section of DNA. Tuesday, CRISPR pioneer Feng Zhang of the Broad Institute at MIT and Harvard reported tweaking the tool’s molecular scissors to significantly lower chances of those “off-target” editing errors – an improvement that could have implications both for developing therapies, and for germline research.
The biggest ethical quandary arises over using those same tools to perform what scientists call “germline” editing, manipulating reproductive cells – sperm, eggs or embryos – to spread gene changes to future generations rather than trying, for example, to fix a defect only in one patient’s blood-producing cells and thus cure his or her sickle cell disease.
In the U.S., germline editing for clinical use – meaning for pregnancy – “is a line that should not be crossed at this time,” John Holdren of the White House Office of Science and Technology Policy said on Tuesday.
Last spring’s experiment in China highlighted that ethics aside, embryo editing wasn’t anywhere near ready for real-world use for safety reasons: Those off-target edits risked fixing one problem only to create another. But there’s controversy over whether and how to continue laboratory experiments to see whether it eventually could work.
Around the world, laws and guidelines vary widely about what germline, or hereditary, research is allowed. Some ban any research; some allow only lab research but not pregnancies; some have no policies. In the U.S., the National Institutes of Health won’t fund germline research but private funding is allowed.
What one country attempts “will have consequences in others,” the White House’s Holdren noted.
Proponents say the ultimate goal is to prevent mom and dad from passing devastating diseases to their children.
“This technology is poised to transform preventive medicine,” Harvard geneticist George Church wrote in Nature.
He added a warning: If mainstream scientists can’t explore heritable gene editing, that “could put a damper on the best medical research and instead drive the practice underground to black markets and uncontrolled medical tourism.”
It’s not just about editing embryos; some potentially simpler treatments hinge on germline editing policies, too. At the University of Pittsburgh, Dr. Kyle Orwig wants to develop treatments for male infertility by altering sperm-producing cells that in some men, don’t do their job.
Doudna adds that a complete ban on such research could block important discoveries. British researchers, for example, plan to alter embryos to study early human development, work that could shed light on miscarriages.
On the other side are critics who argue that standard in vitro fertilization techniques to test the genetics of embryos before they’re implanted, or before adoption, are alternatives. And they raise the specter of parents who can afford designer babies with specific traits.
“The medical arguments are tenuous and the possible social consequences are grave,” said Marcy Darnovsky of the Center for Genetics and Society, an advocacy group.
Online:
Human gene-editing initiative: http://bit.ly/1YDu8OU




